
Design research in a hospital environment is super rewarding. You’ll reveal a wealth of insight and opportunity to improve patient experience but face some unique challenges, especially when interviewing patients at their bedsides.
With a few of these projects under my belt it’s time to share, in case you’re ever in the humbling position to do the same. (yes, more humble pie)
My top tips for patient experience research:
Instinct:
This work will squish everything you’ve got in your soft skill set. You’ll be relying on your instinct for what’s ‘right’ and ‘polite’ in the circumstance. I think doctors call this ‘bedside manner’ …you’re going to need a good one.
Respect and empathy:

Be considerate – happy hour or not.
It goes without saying to be sensitive to this context.
You’re asking people to share their thoughts or story when out of their comfort zone and feeling vulnerable, emotional, philosophical or all of the above. Try to relax patients – make them comfortable, offer to top up their water, pass things, adjust curtains, charge their phone.
Authentic moments:
I prefer to ‘cold call’ on patients at their bedside, inviting them to share their experience on the spot. This lacks the certainty of ‘appointments’ but adds in-the-moment authenticity you simply don’t get if you give people the chance to collect their thoughts and arrange themselves in advance.
Mood-reading:

A chatty, social ward is a good place to find stories.
Each ward or room has it’s own atmosphere, from patients trying to sleep while machines gently beep, through to chat and laughter of visiting families. You’ll need to quickly read the mood and adjust your tone and approach to suit. Pick a lively, social ward and you might find patients are more willing to participate. (but beware of the bias this introduces).
Occupational hazards:
While you’re building empathy for each patient’s circumstance and viewpoint, some of their emotional load will shift to you by osmosis. This is a sign you’re doing a great job of listening, but be ready for emotional exhaustion at the end of each day.
To avoid becoming a patient myself, I start necking immune boosters and vitamin C the week before this work and wash your hands frequently during each day.
Introductions – Staff:
It’s essential ward staff know who you are, and what you’re doing in their working space. I’ve always had a chaperone who’s known and trusted by the staff introduce me and the project objectives. Without this, nurses will be suspicious of who you are and what you’re up to.
Introductions – Patients:
“Hi, I’m Nick, and I’m not a doctor”
Patients will assume you’re clinical staff, a specialist, or coming to discharge them, so get any expectation out of the way as part of your greeting.

Ward staff will point you to the most appropriate patients to talk to, and those to avoid.
Ask staff to suggest which patients are appropriate, and not appropriate to approach. This can save embarrassment for you and patients if they are not completely ‘with it’.
Interviewing:
Maintaining eye contact and looking for non-verbals is essential in this context. You’ll need to record each interview and review later, or bring a note taker.
If it’s your turn to take notes, sketch-noting works very well for feelings, emotions, environmental factors etc. and is super easy to socialise later.

Patients love to see what all that doodling was about, and will elaborate on aspects given the chance.
Here are my top tips for sketch-noting during an interview:
Follow-up:
Ask for permission to interview the patients after discharge in their homes. The in-context interview will be revealing, but you’ll hear a different perspective and mood when they reflect on their in-ward experience.
Kit / recording:
Cameras are an even bigger distraction than usual on a hospital ward, so if you’re filming interviews (and it can be very compelling footage in this context) conceal your camera until you have each patient’s permission to film.
Clear audio is a priority. Patients in a shared ward will tend to whisper out of respect for privacy of others, or so as not to be eavesdropped. Go for a wireless lapel microphone or at least a directional one.
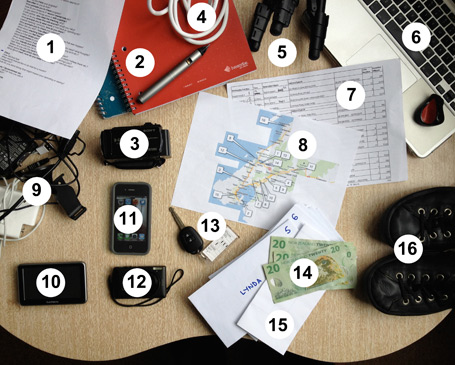
The contents of my hospital kitbag are sparse compared to this lot for home visits. (image from my article in link below)
Check out my article ‘Ethno unpacked – A design researcher’s toolkit‘ for details of the gear I use.
Oh, and one more thing…
SMILE
The more I work in this context, the more I feel like a newbie, and there’s much more to learn.
What have I missed?
What are your experiences?
